Original Editor - Daniel Alcorn as part of the The Jackson Clinics Residency Project
Top Contributors - Daniel Alcorn, Rob Sigler, Kris Porter, Laura Ritchie and Scott Buxton
Contents[hide] |
Links To Diagnostic Imaging Pages
Introduction
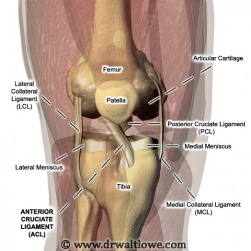
Reprinted from www.drwaltlowe.com
While a thorough history and physical examination are the most important instruments in evaluating knee joint pain, musculoskeletal imaging is an important adjunct.[1] Imaging typically begins with a standard set of plain radiographs, with special radiographic views and more elaborate modalities used if indicated. [1]
Knee Osteoarthritis (OA)
Osteoarthritis (OA) is a multi-factorial condition that is essentially breakdown of hyaline cartilage along articulating joints, and is imaged most often with a radiograph or MRI. Radiographs are the most commonly used source of imaging for knee OA due to their ease of operation, low cost, quick results, and relatively high degree of accuracy. However, an MRI is considered the gold standard for knee OA since articular cartilage is visible and has a much higher resolution of surrounding tissues. There are multiple criteria that are used for OA, but research indicates that these techniques usually have high sensitivity, but at the cost of lower specificity.[2]
Reading Radiograph for Knee OA [2]
• Look for joint narrowing, subchondral sclerosis (increased white/bright location surrounding the joint), and osteophyte formation
Reading MRI for Knee OA [2]
• Fast spin-echo images (ex, fast spin-echo T2-weighted fat-suppressed images) or gradient-echo images (ex, T1-weighted 3-dimensional fat-suppressed images)
• Look for joint narrowing, decreased signal frequency of hyaline cartilage, increased edema and osteophyte formation
• Look for joint narrowing, decreased signal frequency of hyaline cartilage, increased edema and osteophyte formation
Figure 2: Radiograph for knee OA. Reprinted from http://stemcelldoc.wordpress.com/2011/11/16/knee-osteoarthritis-grading-limitations-of-x-rays/
Figure 3: MRI for knee arthritis. Reprinted from http://www.lurj.org/article.php/vol2n1/arthritis.xml
Medial Collateral (MCL) and Lateral Collateral Ligament (LCL) Tears
MCL and LCL tears are classified based on the amount of compartment gapping present with an applied valgus (MCL) or varus (LCL) stress test. Grade I tears present with localized pain along the medial (MCL) or lateral (LCL) knee without significant gapping (0-5 mm). Grade II tears present with significant gapping with a definite endpoint (6-10 mm). Grade III tears (complete) have no defined end point with stress tests (> 10 mm). MCL and LCL tears can be identified with the use of a stress radiograph or MRI (87 % diagnostic accuracy).[3]
Reading stress radiograph for MCL and LCL tears [3]
• Radiographs are performed with the knee in 20 degrees of flexion with comparisons made between the amount of gapping in the injured and uninjured knee

Figure 4: Varus stress radiograph of grade III LCL tear. Reprinted from The Journal of Bone and Joint Surgery.http://jbjs.org/article.aspx?Volume=90&page=2069
Reading MRI for MCL and LCL Tear [3]
• Use of a coronal plane MRI (fast-spin echo T 2 weighted image)
• Look for intermediate signal (consistent with edema), slight thickening and possible retraction of the ligament with possible separation from underlying cortices
• Look for intermediate signal (consistent with edema), slight thickening and possible retraction of the ligament with possible separation from underlying cortices

Figure 5: Grade III medial collateral ligament tear on a coronal fast spin-echo T2-weighted image demonstrates a disrupted ligament that is thickened and retracted, with surrounding edema (black arrow). Reprinted from Medscape Reference.http://emedicine.medscape.com/article/401472-overview
Anterior Cruciate Ligament Tears (ACL)
With a suspected ACL tear, diagnostic imaging first begins with plain radiographs. Commonly, a 45 degree knee flexion, weight-bearing postero-anterior radiograph is obtained to rule out associated fractures and gauge the amount of joint space narrowing. MRI is necessary to diagnose an ACL tear, and is determined using a non-contrast image of the knee.[4]
Reading MRI for ACL tear [5]
• The cruciate ligaments course obliquely through the intercondylar notch and need to be followed on consecutive slices.
• These structures are usually not seen in entirety on one slice, and caution should be exercised in diagnosing a tear on a single slice.
• Look for discontinuity of the ACL in the coronal and sagittal planes
• There are often secondary signs of an anterior cruciate ligament (ACL) injury, such as a joint effusion and bone contusions
• These structures are usually not seen in entirety on one slice, and caution should be exercised in diagnosing a tear on a single slice.
• Look for discontinuity of the ACL in the coronal and sagittal planes
• There are often secondary signs of an anterior cruciate ligament (ACL) injury, such as a joint effusion and bone contusions
Figure 6: Sagittal MRI demonstrating ACL rupture. Reprinted from Sports-Med Forum. http://www.sportsmed-forum.com/index-1/st_pag_patients-home/sm_pag_case-studies-2/sm_pag_case-knee/sm_pag_acl.htm
Meniscus Tears
MRI is utilized to identify the presence of a meniscal tear. The MRI is obtained using a proton-density-weighted, high resolution, fast spin echo sequence (to determine the status of both the articular cartilage and the menisci). Newer MRI techniques, including 3-T scanners with cartilage-sensitive pulse sequences and T 2 mapping, allow detection of early degenerative changes in cartilage before discernible loss of cartilage thickness is visible on a conventional MRI.[6]
Reading MRI for meniscal tear [5]
• Look for areas of abnormal morphology
• Abnormally increased T1 and T2 signals (often linearly orient¬ed) intersect the edges of the meniscus along the articular surface
• Abnormally increased T1 and T2 signals (often linearly orient¬ed) intersect the edges of the meniscus along the articular surface
Figure 7: Coronal T2-weighted fat-saturated fast spin-echo image showing fraying and mild blunting of free edge of body of medial meniscus (large arrow) and horizontal tear of lateral meniscus (small arrow). Reprinted from American Journal of Roentgenology.http://www.ajronline.org/content/187/1/221/F3.expansion.html
Osteochondral Defects
Osteochondral defects (focal areas of articular damage with cartilage damage and injury of the adjacent subchondral bone) are best viewed on MRI. MRI is the test of choice due to its ability to detect the presence of osteochondral fragmentation, which is essential for clinical management. MRI demonstrates high sensitivity (92%) and specificity (90%) in the detection of separation of the osteochondral fragment. Both x-rays and CT are able to detect displaced defects with ease; however they are insensitive in grading lower stage lesions, and are inadequate in predicting stability.[7]
'Reading MRI for osteochondral defects [7]'
• T1 signal is variable with intermediate to low signal adjacent to fragment
• T2 may demonstrate high signal line demarcating fragment from bone (indicating unstable lesion)
• T2 may demonstrate low signal loose bodies, surrounded by high signal fluid
• T2 may demonstrate high signal line demarcating fragment from bone (indicating unstable lesion)
• T2 may demonstrate low signal loose bodies, surrounded by high signal fluid
Figure 8: (A) Osteochondral defect. This coronal T1 sequence shows an area of abnormally low T1 signal in the lateral weight-bearing portion of the medial femoral condyle (arrow), characteristic of osteochondral defect. (B) Osteochondral defect. This sagittal T2 sequence with fat saturation shows subchondral irregularity and heterogeneously low T2 signal with adjacent bone marrow edema in the medial femoral condyle (arrow) characteristic of osteochondral defect. Reprinted from Tall et al.[5]
Subluxation/Dislocation of the Patella
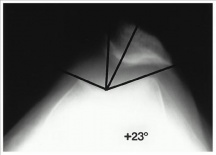
Patellar subluxations and dislocations can be viewed from radiographs, CT scans, or MRI. CT scans are only used in cases in which plain radiographs are indeterminate. MRI can be beneficial to highlight bone bruising (usually on the medial aspect of the patella and lateral aspect of the lateral femoral condyle). [8] The most commonly used imaging technique for these diagnoses is radiography, which usually incorporates a lateral view, axilla view and merchant technique. Images are usually obtained within 20-45 degrees of knee flexion because increased knee flexion results in reduction of a subluxated patella.[8]
Reading Radiograph for patellar subluxation/dislocation [8]
• In a lateral radiograph look for patella alta and/or patellar osteochondral fracture
• In a axilla radiograph look for increased sulcus angle – normal sulcus angle is 137-141
• In a merchant technique look for trochlea dysplasia and an increased congruence angle (compared to the reference sulcus angle from the axilla view)
• Normal congruence angle is defined as < - 16 degrees (negative values indicate medial positioning)
• In a axilla radiograph look for increased sulcus angle – normal sulcus angle is 137-141
• In a merchant technique look for trochlea dysplasia and an increased congruence angle (compared to the reference sulcus angle from the axilla view)
• Normal congruence angle is defined as < - 16 degrees (negative values indicate medial positioning)
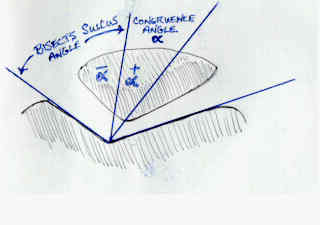
Figure 9: How to calculate congruence angle through the bisection of the sulcus angle. Reprinted from Wheeless CR.[8]
Figure 10: Merchant view radiograph of a lateral patellar subluxation, demonstrating a + 23 degree congruence angle. Reprinted from The Journal of Bone and Joint Surgery. http://jbjs.org/article.aspx?Volume=79&page=1759
References
'- ↑ 1.0 1.1 Berry DJ, Stein mann SP. Adult Reconstruction. Philadelphia, PA: Lipinncott Williams Wilkins, a Walters Kluwer business; 2007: 130-139.
- ↑ 2.0 2.1 2.2 Recht MP, Goodwin DW, Winalski CS, White LM. MRI of articular cartilage: revisiting current status and future directions. AJR. American journal of roentgenology. 2005;185(4):899-914. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16177408. Accessed June 16, 2012.
- ↑ 3.0 3.1 3.2 Laprade RF, Wijdicks CA. The Management of Injuries to the Medial Side of the Knee. Journal of Orthopaedic Sports Physical Therapy. 2012; 42 (3): 221-233.
- ↑ Vyas D, Rabuck SJ, Harner CD. Allograft Anterior Cruciate Ligament Reconstruction: Indications, Techniques, and Outcomes. Journal of Orthopaedic Sports Physical Therapy. 2012; 42 (3): 196-207.
- ↑ 5.0 5.1 5.2 Tall MA, Thompson AK, Greer B, Campbell S. The Pearls and Pitfalls of Magnetic Resonance Imaging of the Lower Extremity. The Journal of Orthopaedic and Sports Physical Therapy. 2011;41(11):873-86.
- ↑ Noyes FR, Heckmann TP, Barber-Westin SD. Meniscus Repair and Transplantation: A Comprehensive Update. Journal of Orthopaedic Sports Physical Therapy. 2012; 42 (3): 274-290.
- ↑ 7.0 7.1 Weerakkody Y, Gaillard F. Osteochondral Defect. Radiopaedia Web site. http://radiopaedia.org/articles/osteochondral-defect. Accessed June 25, 2012.
- ↑ 8.0 8.1 8.2 8.3 Wheeless CR. Subluxation/Dislocation of the Patella. Duke Orthopaedics presents Wheeless’ Textbook of Orthopaedics Web site. http://www.wheelessonline.com/ortho/subluxation_dislocation_of_the_patella. Accessed June 26, 2012.





I have read your blog, really it was very informative and helpful for me having sufficient information about the radiology.
ResponderEliminaryour post is very appreciatable so please keep futher posting. Thank You.diagnostic radiographer.
Thank you for sharing such wonderful information! In my opinion, Keep a healthy life by consuming healthy food and doing exercise regularly is the best healthy formula.
ResponderEliminar