By Scott Baird
www.processmodel.com
I recently performed a process improvement/simulation study of pre op and post op area that serviced a series of surgical suites. I learned a great deal about sizing of the combined system. What had previously been an almost impossible system to understand, with standard operations management tools, became simple with simulation. I analyzed the system and recommended room quantities with a six step simulation model. Because the model was so simple and results applicable to so many people, I wanted to share my success. I hope you find this helpful.
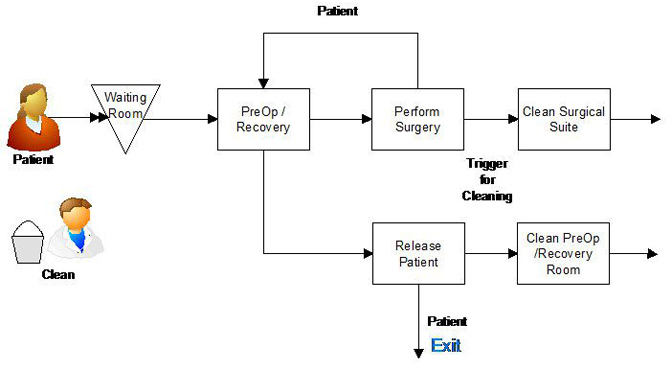
The problem is relatively common. When room is available, patient patients are admitted to a pre op bed. After the pre op work is finished and the surgical suite is ready, the patient is moved to the surgical suite. The pre op bed is reserved for post op recovery. When surgery is completed the patient is returned to the common pre op/post op area. The surgical suite is vacated and signaled for cleaning. When the surgical suite is cleaned it becomes available for use. When the patient completes post op and is discharged, the pre op/post op room is signaled for cleaning. After room cleaning the pre op/post op area can admit another patient.
The trick to calculating the size of the pre op/post op and surgical suites is threefold. First, none of the times are a single number. Times for pre-op, post op/recovery and cleaning are variable. I have learned from past experience that using averages to calculate throughput is about as accurate as diagnosing a patient with a picture. Second, there are limited cleaning resources. If multiple rooms or surgical suites become available for cleaning at exactly the same time, there is a delay waiting for the cleaning resource finish the rooms in sequence. Third, pre op and post op are the same room. Once a room is occupied by a patient it is not released until that patient finishes post op and the room is cleaned. Yikes…the calculations were impossible.
I tried using averages and a spreadsheet to mimic an existing hospital system, but I couldn’t even come close to matching the behavior of the real system. I had watched an associate perform a process improvement project with simulation and recognized that this was a perfect fit. I had a complex system, lots of variability and interdependencies between pre and post op.
The simulation model simple to develop. Most of what I needed came from examples on the vendor’s website. I had to develop and enter: patient arrivals; distributions for pre op, surgery, post op, and room cleaning times. The basic flow of the simulation model is show below:
The software I used is called ProcessModel. The logic for handling availability of the pre op/recovery rooms and surgical suites was provided in the vendor examples. It took two days to prepare our data and validate the behavior of the model.
Once I entered the data, the simulation software allowed a definition of a target (which was waiting time for our hospital). The software automatically ran through an optimization routine to calculate the number of pre op/recovery rooms, surgical suites and cleaners to hit the defined target. This is the only time that I have been able to allow the computer to perform unsupervised process improvement (I actually went to lunch). I later verified the optimized process by watching the animated simulation model over a period of simulated months. I had to make a couple of adjustments but the automated optimization was effective.
As mentioned in the opening paragraph, is the first time that I have used simulation to perform a process design/process improvement study. I found that the doctors were skeptical at first, but became very attentive and participative after they understood how the model worked. On hindsight, I should have introduced the simulation software on an example out of their area expertise at the start of the project. This pre-introduction would have saved several hours of explanation. I also found that using the simulation modeling software to mimic an existing system in the hospital (that could verified) was instrumental in gaining confidence and acceptance from the doctors. I am excited to compare the real system with the model in the near future. Based on the existing system that we modeled to validate our methods, I have confidence that the model will be close to reality.
Sem comentários:
Enviar um comentário
Gostou do meu Blog? Envie a sua opinião para lmbgouveia@gmail.com