History
The type of graft that the surgeon chooses for ACL reconstruction has evolved over the past few decades. In the 1970s, Erickson popularized the patellar tendon graft autograft that Jones had originally described in 1960. This became the most popular graft choice for the next three decades. In fact, in a survey of American Academy of Orthopaedic Surgeon members done in 2000, 80% still favored the use of the patellar tendon graft.
In the light of harvest site morbidity and postoperative stiffness associated with the patellar tendon graft, many surgeons began to look at other choices, such as semitendinosus grafts, allografts, and synthetic grafts. Fowler and then Rosenberg popularized the use of the semitendinosus. However, even Fowler was not convinced of the strength of the graft. Then, Kennedy and Fowler developed the ligament augmentation device (LAD) to supplement the semitendinosus graft. Gore-Tex (Flagstaff,AZ), Leeds-Keio, and Dacron (Stryker, Kalamazoo, MI) were choices for an alternative synthetic graft to try to avoid the morbidity of the patellar tendon graft. The initial experience was usually satisfactory, but the results gradually deteriorated with longer follow-up.
Allograft was another choice that avoided the problem of harvest site morbidity. The initial allograft that was sterilized with ethylene oxide had very poor results. Today the freeze-dried, fresh-frozen, and cryopreserved are the most popular methods of preservation of allografts.
The allograft has become a popular alternative to the autograft because it reduces the harvest site morbidity and operative time. However, Noyes has reported a 33% failure with the use of allografts for revision ACL reconstruction.
The aggressive postoperative rehabilitation program advocated by Shelbourne in the 1990s greatly diminished the problems associated with the patellar tendon graft. Before that, the patient had to be an athlete just to survive the operation and rehabilitation program. Theaggressive program emphasized no immobilization, early weight bearing, and extension exercises.
There was renewed interest in the semitendinosus during the mid-1990s. Biomechanical testing on the multiple-bundle semitendinosus and gracilis grafts demonstrated them to be stronger and stiffer than other options. This knowledge combined with improved fixation devices such as the Endo-button gave surgeons more confidence with no-bone, soft tissue grafts. The Endo-button made the procedure endoscopic, thereby eliminating the need for the second incision. Fulkerson, Staubli, and others popularized the use of the quadriceps tendon graft. This again reduced the harvest morbidity, especially when only the tendon portion was harvested.
Shelbourne has described the use of the patellar tendon autograft from the opposite knee. He claims that this divides the rehabilitation between two knees and reduces the recovery time. With the contralateral harvest technique, the average return to sports for his patients was four months. With both the patellar tendon and the semitendinosus added to the list of graft choices, the need for the use of an allograft is minimized.
The latest evolution is to use an interference fit screw to fixate the graft at the tunnel entrance. This produces a graft construct that is strong, short, and stiff. It means that the surgeon now has to learn just one technique for drilling the tunnels and can chose whatever graft he or she wishes: hamstring, patellar tendon, quadriceps tendon, or allograft.
Successful ACL reconstruction depends on a number of factors, including patient selection, surgical technique, postoperative rehabilitation, and associated secondary restraint ligamentous instability. Errors in graft selection, tunnel placement, tensioning, or fixation methods may also lead to graft failure. Comparative studies in the literature show that the outcome is almost the same regardless of the graft choice. The only significant fact from the metaanalysis, as confirmed by Yunes, is that the patellar tendon group had an 18% higher rate of return to sports at the same level. The most important aspect of the operation is to place the tunnels in the correct position. The choice of graft is really incidental. Studies by Aligetti, Marder, and O’Neill show that the only significant differences among the grafts is that the patellar tendon graft has more postoperative kneeling pain.
Evolution in Graft Choice at Carleton Sports
Medicine Clinic
The most popular graft in the early 1990s was the patellar tendon graft
(Fig. 1). With the evolution of the 4-bundle graft and improved fixation in the mid-1990s, the hamstring graft became more popular. The swing to hamstring grafts then became largely patient driven.When the patients went to therapy after the initial ACL injury, they saw how easy the rehabilitation was for the hamstring tendon and opted for that graft.
The main choices of graft for ACL reconstruction are the patellar tendon autograft, the semitendinosus autograft, and the central quadriceps tendon, allograft of patellar tendon, Achilles tendon, or tibialis anterior tendon, and the synthetic graft.
Figure 1. The evolution of the graft choice. The white bar is the hamstring graft.
Patellar Tendon Graft
The patellar tendon graft was originally described as the gold-standard graft. It is still the most widely used ACL replacement graft (i.e., it is used in approximately 80% of cases), but it is not without problems. Shelbourne has pushed the envelope further with the patellar tendon graft. He has recently reported on the harvest of the patellar tendon graft from the opposite knee, with an average return to play of four months postoperative.
The advantages of the patellar tendon graft are early bone-to-bone healing at six weeks, consistent size and shape of the graft, and ease of Patellar Tendon Graft harvest. The disadvantages are the harvest site morbidity of patellar tendonitis, anterior knee pain, patellofemoral joint tightness with late chondromalacia, late patella fracture, late patellar tendon rupture, loss of range of motion, and injury to the infrapatellar branch of the saphenous nerve. Most of the complications are the result of the harvest of the patellar tendon.This is still the main drawback to the use of the graft.
Patellar Tendon Graft Indications
The ideal patient for an ACL reconstruction is the young, elite, competitive, pivotal athlete. This is the young athlete who wants to return to sports quickly and is going to be more aggressive in contact sports for a longer period of time. There is no upper age limit for patellar tendon reconstruction, but the younger athlete has more time to commit to knee rehabilitation. If the patellar tendon is the gold standard of grafts, then this is the graft of choice for the professional, or elite, athlete. Finally, the competitive athlete understands the value of the rehabilitation program and will not hesitate to spend three hours a day in the gym. The author’s assessment is that 50% of the success is the operation, and 50% is the rehabilitation program.
Pivoting Activities
The ACL is only required for pivotal athletics. Most nonpivotal athletes can usually cope without an ACL. Cyclists, runners, swimmers, canoeists, and kayakers, for example, can function well in their chosen sport without an intact ACL.
Athletic Lifestyle
This operation should be reserved for the athletic individual. In most activities of daily living the ACL is not essential. If the nonathlete has giving way symptoms, it is probably the result of a torn meniscus and not a torn ACL.The meniscal pathology can be treated arthroscopically, and the patient can continue with the use of a brace as necessary.
Patellar Autograft Disadvantages
Harvest Site Morbidity
The main disadvantage of the patellar tendon graft is the harvest site morbidity. The problems produced by the harvest are patellar tendonitis, quadriceps weakness, persistent tendon defect, patellar fracture, patellar tendon rupture, patellofemoral pain syndrome, patellar entrap-ment, and arthrofibrosis. The common long-term problem is kneeling pain.
Kneeling Pain
The most common complaint after patellar tendon harvest is kneeling pain. This can be reduced by harvesting through two transverse incisions. This reduces the injury to the infrapatellar branch of the saphenous nerve.
Patellar Tendonitis
Pain at the harvest site will interfere with the rehabilitation program. The strength program may have to be delayed until this settles. The problem is usually resolved in the first year, but it can prevent some high performance athletes from resuming their sport in that first year.
Quadriceps Weakness
The quads weakness may be the result of pain and the inability to participate in a strength program. If significant patellofemoral symptoms develop, the athlete may be unable to exercise the quads.
Persistent Tendon Defect
If the defect is not closed, there may be a persistent defect in the patellar tendon. This results in a weaker tendon.
Patella Entrapment
If the defect is closed too tight, the patella may be entrapped, and patellar infera may result. This will certainly result in patellofemoral pain, because of an increase in patellofemoral joint compression.
Patella Fracture
The fracture may occur during the operation or in the early postoperative period. Intraoperative patella fracture may be the result of the use of osteotomes. If the saw cuts are only 8-mm deep and 25-mm long, and the base is flat to avoid the deep V cut, an intraoperative fracture is rare. The late fractures are produced by the overruns of the saw cuts. The overruns may be prevented by cutting the proximal end in a boat shape.
The left X-ray shows a displaced transverse patellar fracture, at three months postoperative. The right X-ray shows the postoperative internal fixation with cannulated AO screws and figureof-eight wire.
Figure 2. X-ray of displaced transverse patellar fracture at three months postoperative.
Figure 3. X-ray of postoperative internal fixation with cannulated AO screws and figure-of-eight wire
Tendon Rupture
This may occur if a very large graft is taken from a small tendon. The standard is a 10-mm graft, measured with a double-bladed knife. The bone blocks are trimmed to 9 mm to make the graft passage easier.
Patellofemoral Pain
This topic is controversial in the literature. The older literature reported a high incidence of patellofemoral pain associated with ACL reconstruction. However, most of the disability could be blamed on rehabilitation programs that consisted of immobilization.There is no doubt that some patients will develop pain, some will develop crepitus, and some will have tendonitis, but results have improved with more aggressive rehabilitation programs with early motion and weight bearing. To prevent the patella from being bound down, the patella should be mobilized daily by the physiotherapist.
Arthrofibrosis
This severe problem is rarely seen now in ACL reconstructions.The true condition is idiopathic and is probably the result of fibroblastic proliferation. As a result, very little can be done to prevent it. It may be more common in the patient who forms keloid. The more common condition of loss of range of motion may be the result of incorrect tunnel placement or postoperative immobilization. In the mid-1980s, a limited range of motion hinge cast (preventing 30° of extension) was used for six weeks postoperatively, thereby causing problems in regaining extension. Many of these cases required arthroscopic debridement (10–18%, in the first year). The loss of extension was almost completely eliminated by changing to an extension splint. The acceptance of aggressive physiotherapy to regain extension eliminated the problem. This problem of postoperative stiffness made the use of a synthetic ligament, with no immobilization, very attractive. The reoperation for loss of range of motion is now very uncommon.
Tendon Rupture
This may occur if a very large graft is taken from a small tendon. The standard is a 10-mm graft, measured with a double-bladed knife. The bone blocks are trimmed to 9 mm to make the graft passage easier.
Patellofemoral Pain
This topic is controversial in the literature. The older literature reported a high incidence of patellofemoral pain associated with ACL reconstruction. However, most of the disability could be blamed on rehabilitation programs that consisted of immobilization.There is no doubt that some patients will develop pain, some will develop crepitus, and some will have tendonitis, but results have improved with more aggressive rehabilitation programs with early motion and weight bearing. To prevent the patella from being bound down, the patella should be mobilized daily by the physiotherapist.
Arthrofibrosis
This severe problem is rarely seen now in ACL reconstructions.The true condition is idiopathic and is probably the result of fibroblastic proliferation. As a result, very little can be done to prevent it. It may be more common in the patient who forms keloid. The more common condition of loss of range of motion may be the result of incorrect tunnel placement or postoperative immobilization. In the mid-1980s, a limited range of motion hinge cast (preventing 30° of extension) was used for six weeks postoperatively, thereby causing problems in regaining extension. Many of these cases required arthroscopic debridement (10–18%, in the first year). The loss of extension was almost completely eliminated by changing to an extension splint. The acceptance of aggressive physiotherapy to regain extension eliminated the problem. This problem of postoperative stiffness made the use of a synthetic ligament, with no immobilization, very attractive. The reoperation for loss of range of motion is now very uncommon..
Contraindications to Harvest of the Patellar Tendon
Preexisting Patellofemoral Pain
Is preexisting patellofemoral pain a contraindication to harvesting the patellar tendon? The conventional wisdom is yes; it would not be a wise procedure in this situation. Rather, it is like hitting a sore thumb with a hammer! In the past, when chondromalacia was seen at the time of arthroscopy, the graft choice would be changed to hamstrings.
The Small Patellar Tendon
The harvesting of the central third of the patellar tendon in a small tendon is more theoretical than practical. The advice in a small patient with a tendon width of only 25 mm would be to take a narrower graft of 8 to 9 mm or use another graft source.
Preexisting Osgoode-Schlatters Disease Shelbourne has reported that a bony ossicle from Osgoode-Schlatters disease is not a contraindication to harvest of the patellar tendon.
Because the fragment usually lies within the bony tunnel, this bone may be incorporated into the tendon graft.
Hamstring Grafts
Advantages of Hamstring Grafts
The main advantage of the hamstring graft is the low incidence of harvest site morbidity. After the harvest, the tendon has been shown by MRI to regenerate. The 4-bundle graft is usually 8mm in diameter, which is a larger cross-sectional area than the patellar tendon.
Disadvantages of Hamstring Grafts
The disadvantage of any autograft is the removal of a normal tissue to reconstruct the ACL. The harvest of the semitendinosus seems to leave the patient with minimal flexion weakness. One study did show some weakness of internal rotation of the tibia after hamstring harvest.
Injury to the saphenous nerve is rare and can be avoided with careful technique. The fixation of the graft remains one of the controversial issues.
Issues in Hamstring Grafts
The major issues with the use of hamstring grafts are:
Graft strength.
Graft fixation.
Graft healing.
Donor site morbidity.
Early rehabilitation.
Graft strength and stiffness.
In one of the earlier studies, Noyes reported that one strand of the semi-t was only 70% the strength of the ACL. However, hecompared this to a 15-mm-wide patellar tendon graft that was 125% the strength of the native ACL. This was widely quoted as a reason to use the patellar tendon graft rather than the hamstring.With the advent of the multiple bundles of hamstrings, this graft now has twice the strength of the native ACL (Fig. 7). Sepaga later reported that the semitendinosus and gracilis composite graft is equal to an 11-mm patellar tendon graft. Marder and Larson felt that if all the bundles are equally tensioned, the double-looped semi-t and gracilis is 250% the strength of the normal ACL. Hamner, however, emphasized that the strength is only additive if the bundles are equally tensioned.
Soft Tissue Fixation Techniques
There are various techniques for securing the soft tissue to the bony tunnel in ACL reconstruction. Each one has strengths and weaknesses. Pinczewski pioneered the use of the RCI interference fit metal screw for soft tissue fixation. The use of a similar type of bioabsorbable screw that was used in bone tendon bone fixation was a natural evolution. To overcome the weak fixation in poor quality bone, the use of a round pearl, made of PLLA or bone, was developed.This improved the pullout strength by 50%.The Endo-button, popularized by Tom Rosenberg, was improved with the use of a continuous polyester tape. This made the fixation stronger and avoided the problems of tying a secure knot in the tape. The cross-pin fixation has proven to be the strongest, but has a significant fiddle factor to loop the tendons around the post. The Arthrex technique is the easiest to use.Weiler, Caborn, and colleagues have summarized the current concepts of soft tissue fixation. The estimates of the force on the normal ACL during activities of daily living are as follows:
Level walking: 169N
Ascending stairs: 67N
Descending stairs: 445N
Ascending ramp: 27N
Descending ramp: 93N
It is commonly quoted that a person needs more than 445N pullout strength of the device just to handle the activities of daily living. However, Shelbourne has reported good results with the patellar tendon graft fixed by tying the leader sutures over periosteal buttons (Ethicon, J&J, Boston, MA). This form of fixation has a low failure strength, but is clinically successful. The gold standard of the interference fit screw fixation of the bone tendon bone, 350 to 750N, has been used to compare the soft tissue fixation.
The pullout strengths also vary from tibia to the femur. The femoral pullout is higher because the tunnel is angled to the graft and the pull is against the screw that is placed endoscopically. In the tibial tunnel, the graft pulls away from the screw in the direct line of the tunnel.
The initial fixation points were at a distance from the normal anatomical fixation of the ACL. The trend has been to move the fixation closer to the internal aperture of the tunnel. This shortening of the intraarticular length has improved the stiffness of the graft.
The pullout strength of bioabsorbable screw can vary widely depending on its composition. The screw fixation has also been shown to be bone quality dependent. These considerations should be taken into account when choosing a femoral fixation device for soft tissue grafts.
Disadvantages
The disadvantages of the hamstring graft are the various methods used to fix the graft to bone, including staples, Endo-button, and interference fit screws. Furthermore, the graft harvest can be difficult, the tendons can be cut off short, and there is a longer time for graft healing to bone, approximately 10 to 12 weeks.
Pullout Strengths of Soft Tissue Devices
The fixation of the graft depends on both the tibial and femoral fixation. The rehabilitation protocol should reflect the type of fixation used. All the femoral fixation devices provide reasonable fixation. The cyclic load is more important than the ultimate load to failure. The interference screw fares worst with cyclic loads.
Interference Fit Screws
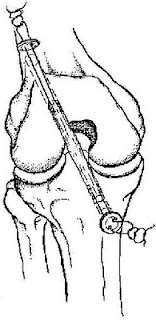
The interference fit screw is shown is Figure 4.
Figure 4. The interference screw fixation of the soft tissue graft in a cadaver model
.
Advantages
The advantages are as follows:
Quick, familiar, and easy to use.
Direct bone to tendon healing, with Sharpey’s fibers at the tunnel aperture.
Less tunnel enlargement.
Disadvantages
The disadvantages are as follows:
Longer graft preparation time.
Bone quality dependent.
Damage to the graft with the screw.
Divergent screw has poor fixation.
Removal of metal screw makes revision difficult.
Several refinements have been made to the interference screw technique to increase the pullout strength and cyclic load performance. The end of the graft may be backed up with a round ball of PLLA, the Endo- Pearl (Linvatec, Largo, FL) or bone to abut against the screw and prevent the slippage of the graft under the screw. The tunnels may be dilated or compacted when the bone is osteopenic.A longer screw with a heavy whipstitch in the graft improves pullout strength. The leader sutures from the graft may be tied over a button or post on the tibial side to back up the screw fixation.
Cross-Pin Fixation
The cross-pin fixation is shown in Figure 5
Figure.5. The Arthrex transfix pin fixation of soft tissues.
Advantages
The advantages are as follows:
Strongest tested fixation.
May individually tension all bundles of graft.
Disadvantages
The disadvantages are as follows:
Pin may tilt in soft bone and lose fixation.
Steep learning curve of fiddle factor.
Special guides are required.
Buttons
Buttons are shown in Figure 6 and Figure 7.
Figure 6. The Endo-button periosteal cortical femoral fixation of hamstring grafts.
Figure 7 The periosteal button fixation of soft tissue grafts.
Advantages
The advantages are as follows:
The Endo-button with closed loop tape is strong, if expensive.
The plastic button is cheap, available and easy to do.
Disadvantages
The disadvantages are as follows:
Fixation site is distant with increase in laxity, with the bungee cord effect.
Increased in tunnel widening.
Plastic button has low pullout strength, dependent on the sutures.
Tibial Fixation
The tibial fixation remains a problem with soft tissue graft fixation. Patients generally do not tolerate metal devices in the subcutaneous area on the front of the tibia. The interference screw gets away from that problem, but has poor performance in cyclic load. The graft tends to slip out from under the screw as the knee is cycled. A backup fixation must be used it the interference screw is used. The Intrafix (Mitek) device uses the interference screw fixation principle, but increases both the ultimate load to failure and the cyclic load performance.
Considerations
The most important consideration in ACL reconstruction is that the tunnels are put in the correct position. After this, the fixation of the graft is the next most important factor in a satisfactory clinical outcome. The physician should become proficient at one of these techniques. For revi-sions, physicians may need to have available another type of fixation to deal with hardware and tunnel expansion.
Tendon-to-Bone Healing
Studies have shown that it takes at least 8 to 12 weeks for soft tissue to heal to bone, as compared to 6 weeks for bone-to-bone healing with the patellar tendon graft. Recent studies have shown that the compression of the tendon in the tunnel with a screw speeds the time of healing, similar to internal compression in bone healing.
Donor Site Morbidity
In 1982, Lipscomb found that after harvest of the semitendinosus only the strength of the hamstrings was 102% and after harvest of both the strength was 98%. Recently, it has been shown that the internal rotation strength is decreased after the harvest of the semitendinosus. The patellofemoral pain incidence has been reported by Aligetti to be 3 to 21% after semitendinosus reconstruction. There are rare reported cases of saphenous nerve injury.
Early Rehabilitation
Prospective randomized studies by Aligetti and Marder have shown that with early and aggressive rehabilitation, there was no difference between the semitendinosus and patellar tendon grafts in stability or final knee rating. This puts to rest the argument as to whether the hamstring graft can withstand early aggressive rehabilitation protocols.
Central Quadriceps Tendon
This graft has been largely ignored in North America over the past decade. An assistant can harvest the graft while the surgeon is doing the notchplasty. It is a large diameter graft, 10 ¥ 10mm (Fig. 5.12). The tendon graft is fixed with interference screws for the bone plug and sutures tied over buttons for the tendon end. A bioabsorbable interference screw may be used at the internal aperture of the tunnel to reduce the tendon motion in the tunnel. The quadriceps tendon graft should reduce the need for the allograft or synthetic in revision cases.
Figure. 8 The quadriceps tendon graft.
Allografts
Advantages
The allograft has no harvest site morbidity. With no harvest required, the time of the operative procedure is reduced.
Disadvantages
The main objection to the use of the allograft is the risk of disease transmission. Jackson has shown that it takes longer for the graft to incorporate and mature, meaning a longer time until the patient can return to sports. In addition, there is a limited availability of allograft materials. In the literature, Noyes has shown that in long-term follow-up, failure rates increase. In the 1997 survey of the ACL study group by Campell, none of the members used allografts for primary reconstructions.
Synthetic Grafts
The best scenario for the use of the LARS synthetic graft is when the graft can be buried in soft tissue, such as in extra-articular reconstruction. This allows for collagen ingrowth and ensures the long-term viability of the synthetic graft. It will be sure to fail early if it is laid into a joint bare, especially going around tunnel edges, and is unprotected by soft tissue.
Advantages
There is no harvest site morbidity with the use of the synthetic graft. The graft is strong from the time of initial implant. There is no risk of disease transmission.
Disadvantages
The main disadvantage is that all the long-term studies have shown high failure rate. There is the potential for reaction to the graft material with synovitis, as seen with the use of the Gore-Tex graft.With the Gore-Tex graft, there was also the increased risk of late hematogenous joint infection. The results that have been reported with the use of the Gore-Tex graft suggest that it should not be used for ACL reconstruction. Unacceptable failure rates have also been reported with the use of the Stryker Dacron ligament and the Leeds-Keio ligament. The ligament augmentation device was also found to be unnecessary.
Figure 9 The insertion of the BioScrew through the anteromedial portal
Figure 10. The insertion of the BioScrew into the femoral tunnel